
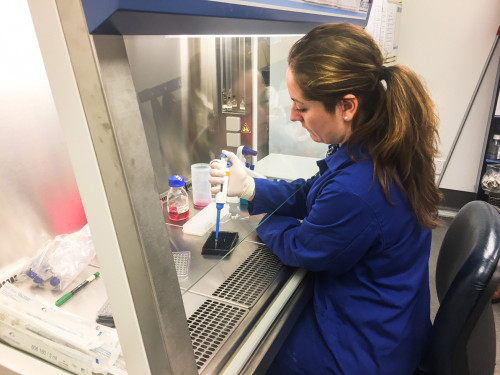
Professor Kathryn Stowell and Sophie Burling
Organ-on-a-chip technology to tackle a rare disorder
New technology being developed as part of a SfTI research project, could provide an alternative to painful biopsies used to diagnose a rare and potentially fatal neuromuscular disorder – malignant hyperthermia.
The disease causes a catastrophic metabolic reaction when someone with genetic MH-susceptibility is given an inhalational anaesthetic. Such reactions are rare – estimated at 1 in 15,000 for children and 1 in 50,000 for adults.
Since 1986 diagnosis has involved taking a large biopsy of a patient’s muscle tissue. But it can be a painful process and isn’t available to children under the age of 12 or for the elderly, who may have reduced muscle mass.
Prior diagnosis is critical as reactions can prove fatal unless an antidote is quickly administered. The Manawatu-Horowhenua area has unusually high prevalence of the disorder, due to a large family being affected, the first in New Zealand to be diagnosed with MH-susceptibility.
“It means that at Palmerston North Hospital, one in every 175 surgeries would need to be treated as MH susceptible,” says Massey University’s Professor Kathryn Stowell, a biochemist who has developed DNA tests for the genetic disorder at Massey’s lab.
A solution to painful and invasive biopsies
Genetic testing for MH is problematic because there are hundreds of genetic mutations associated with it, and only half of the over 60 families throughout New Zealand can currently be offered genetic testing. A better way of testing for and diagnosing MH was needed and the potential solution came from Massey PhD student Sophie Burling.
“I was looking for technologies to bridge that gap between what is happening in a human and what's happening in the lab,” says Burling, who studied MH as part of her honours degree.
Growing human tissue in the lab
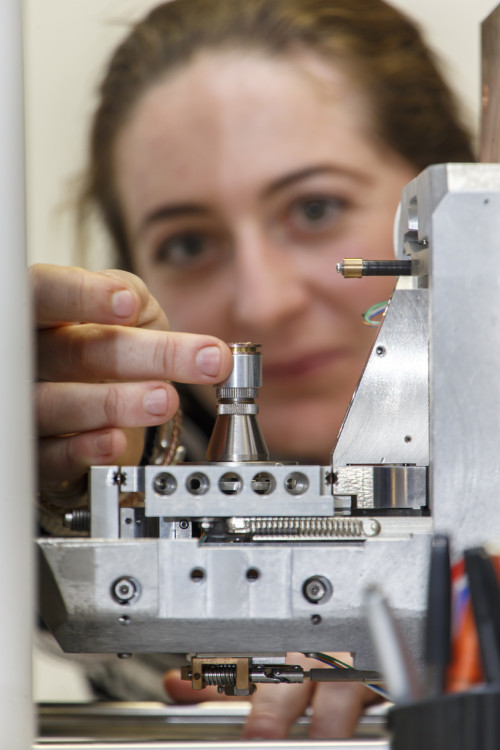
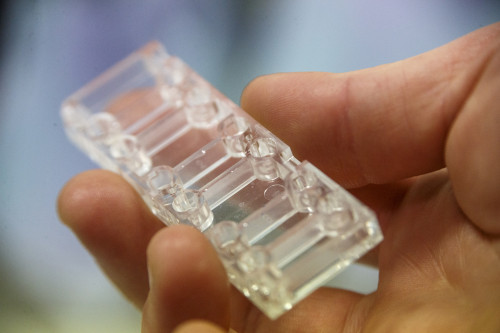
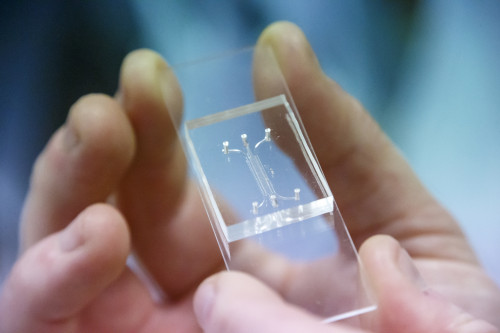
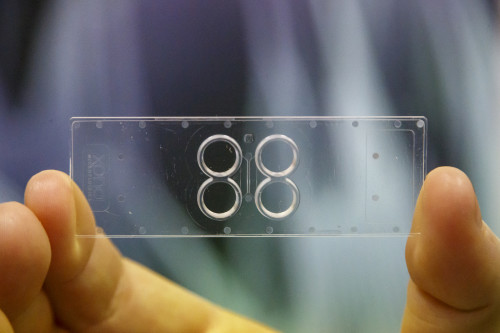
Burling looked at devices being used overseas to grow human tissue and even organs in the lab. She then set about using the technology to cultivate muscle tissue and motor neurons derived from the cells of MH sufferers as well as healthy patients.
A two-year Science for Technological Innovation 2019 Seed project will now see Burling, and a comprehensive team of experienced researchers attempt to develop a reliable diagnostic test for MH in the lab as an alternative to the biopsies.
“We are able to reprogramme cells to become stem cells, which allows us to then create motor neurons and muscle tissue specific to each patient,” says Burling.
Early progress had seen her able to generate human muscle that can contract, a crucial requirement to perform a diagnostic of this nature.
Diagnosis solution for a multitude of neuromuscular disorders
The researchers are confident the technology could be used for less invasive diagnosis of a range of neuromuscular disorders as well as ongoing research into the nature and treatment of these devastating diseases. But the immediate benefit would come to those, who currently cannot be offered genetic testing, seeking to discover if they carried the genetic defect that leads to MH-susceptibility.
“Instead of having to spend a day in hospital for a biopsy, they can pull some hairs or give some blood which we can use to create their cells in the lab,” Burling explains.
“Using this miniaturised technology, we can create a synthetic emulation of an actual patient.”
Innovation collaboration across NZ and Australia
Burling will work with collaborators outside of the team of Massey University researchers including Dr Deanne Whitworth, an expert in cell reprogramming at the Australian Institute for Bioengineering and Nanotechnology and Dr Volker Nock, a specialist in microfabrication and on-chip technologies based at the University of Canterbury. These collaborations will prove instrumental to the Seed project which will run through to the middle of 2021.
Top image: Professor Kathryn Stowell and PhD student, Sophie Burling in Massey University School of Fundamental Sciences Lab.