
Professor Richard Haverkamp
Scaffolding with collagen
If you take an artery from any animal at the freezing works and remove the blood, muscle and other tissues, you’ll be left with collagen. And that collagen is chemically the same as what’s found in your own bones, muscles, skin and tendons – it’s the most abundant protein you have.
SfTI Seed researcher Professor Richard Haverkamp is capitalising on that universality in his work to examine the potential of collagen from animals as a support for damaged structures within the human body while they’re under natural repair.
“There’s a lot of companies that make collagen for surgical repair in sheet form, and you’d see that used in skin grafts, for example. They do that by dissolving out the collagen and then reconstructing it to look a bit like a piece of tissue paper,” Richard says.
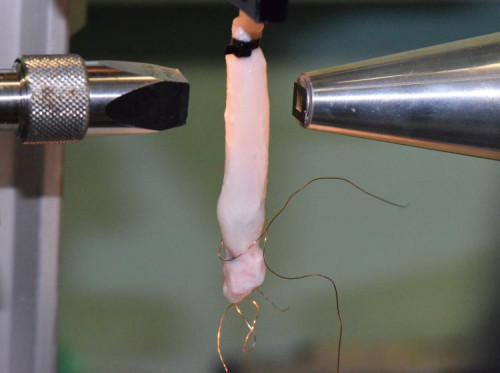
“So if you have some damage in the body, like a severed nerve or weakened artery wall, our thought is that it would be useful to be able to slide a collagen sleeve around the damage to support the body while it’s repairing the structure – a bit like scaffolding.
“Veins and arteries actually come pre-formed into the right straw shape for that, so it makes sense to use those rather than taking flat-sheet collagen and trying to form it into tubes.”
“Veins and arteries actually come pre-formed into the right straw shape...”
Richard is working with postdoctoral fellow Hannah Wells and Professor Chris Cunningham to prepare this tubular collagen in a different way – removing the non-collagen cells and leaving only a scaffold of collagen behind.
“They’ll be stiff when dry, so potentially quite easily transportable, and could come in an unlimited range of sizes, from very thin capillary-sized sleeves to something that could surround and support your aorta.”
Richard says the initial focus will be to study the behaviour of the collagen scaffolds in various circumstances.
“An important one is to observe it under pressure, which is what it will face in the body. We’ll be inflating the structures with air to the pressure ranges found in human blood pressure to understand whether that causes any changes.
“This will affect the collagen fibrils which make up the scaffold. If you imagine taking a white worm, with bands running around it at intervals, but at the scale of 60 nanometers, that is what a collagen fibril looks like. Then when we do things to the scaffold, like stretching it long-ways and inflating it, we can see how the collagen responds. One of the tools we use to do this is the Australian Synchrotron. We want to produce accurate measurements of what’s happening at a nanoscale to the collagen when you do those things.
“The medical world knows how flat sheets of collagen tissue behave, but that’s not necessarily how the same type of material will behave in a different shape.”
Richard says there’s already some commercial interest in the work, which would need to undergo extensive approvals before being available for use in humans.
“But we think the idea has a lot of promise. The other advantage is that this material is ethical. It doesn’t involve dedicated killing of animals, but rather just harvesting material that would otherwise be thrown out as waste.”
Top image: Post doctoral fellow Hannah Wells and Professor Richard Haverkamp with a freeze drier used in the preparation of the scaffolds.